What is Diabetic Retinopathy?
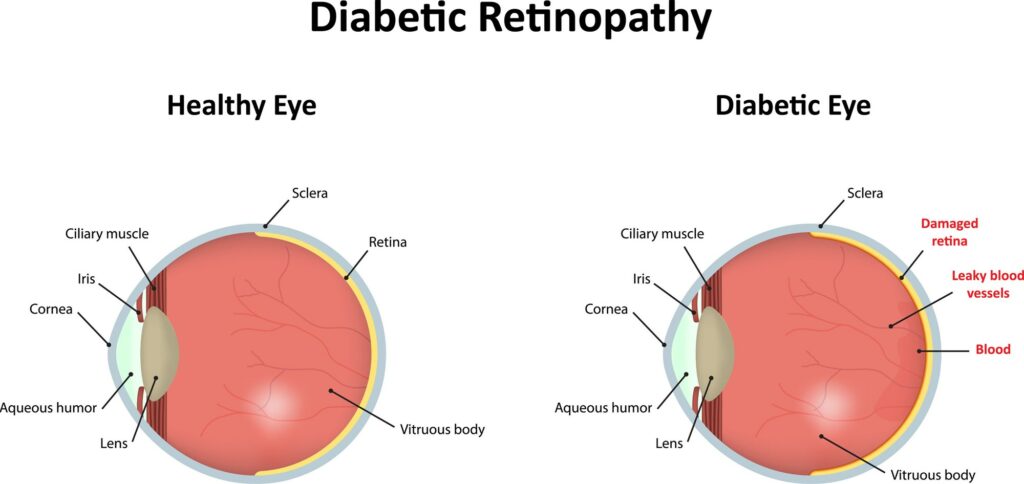
Diabetic retinopathy can develop when a patient living with type 2 diabetes has high blood sugars that damage the blood vessels in the retina, a part of the eye that’s critical to helping the brain form images that help make sense of the visible world.
There are two types of diabetic retinopathy: nonproliferative and proliferative.
In nonproliferative diabetic retinopathy, high blood sugars lead to a weakening of the walls of the blood vessels in the retina.
In proliferative diabetic retinopathy, the injured blood vessels eventually stop working, and new blood vessels form. But these new blood vessels don’t work very well either, as they can be prone to leaking. The growth of these new blood vessels can lead to the retina becoming detached, which can lead to other vision problems, including vision loss. These newly-formed blood vessels can increase the risk of developing glaucoma as well.
Diabetic retinopathy can cause a range of symptoms, whether it’s blurry vision, an inability to distinguish between colors, or vision loss. But symptoms generally don’t emerge very quickly, which is why patients living with diabetes are advised to see an ophthalmologist on a regular basis for eye exams that can help detect the presence of diabetic retinopathy.
Why diabetic retinopathy is dangerous
Many people aren’t aware they have diabetic retinopathy until it has moved from early stages (nonproliferative retinopathy) to a point when leaking blood vessels break open and cause scar tissue that can pull on the retina (proliferative retinopathy). A delayed or lack of treatment can make it very difficult to maintain vision.
Diabetic retinopathy symptoms
The condition is often asymptomatic, especially in early cases. But as it progresses, effects are pronounced — including a lessened (or lost) ability to read or drive. Gardner says patients also may start “seeing blood floating around in their eyes” in the form of tiny black or red dots.
How diabetic retinopathy is diagnosed
Patients should notify a doctor if symptoms arise, but dilation during a routine eye exam can offer clues. Most commonly, small hemorrhages in the back of their eye are indications of this condition worsening. Another sign is swelling of the retina or growth of abnormal blood vessels.
Who is at risk of diabetic retinopathy?
People with type 1 and type 2 diabetes generally have the same likelihood of developing diabetic retinopathy. African Americans and Hispanics have a higher overall risk. Secondary factors like foot infections, anemia or coexisting kidney disease can all contribute to diabetic retinopathy.
How diabetic retinopathy is treated
Steroids and medications known as anti-vascular endothelial growth factor (anti-VEGF) can help. Steroids reduce inflammation, and the anti-VEGF drugs inhibit the action of a specific molecule inside the eye that promotes leaking blood vessels — and the formation of abnormal new ones. Depending on severity, some patients may be advised to receive laser eye treatment.
Ways to prevent diabetic retinopathy
Not everyone with type 2 diabetes will develop diabetic retinopathy. But for folks living with type 2 diabetes, keeping blood sugars under control can help prevent severe vision loss, and even slow progression of retinopathy. Quitting smoking can also help lower one’s risk, as can keeping one’s blood pressure in a healthy range. In the event that severe diabetic retinopathy develops, a number of treatments can help. The optimal treatment option is chosen based on the specific features of one’s retina.